In a large cohort of patients with type 2 diabetes, multidisciplinary care in a primary care setting was associated with a lower risk of all-cause dementia, including a 39% lower risk of vascular dementia and a 29% lower risk of other subtypes. was associated with a 28% lower risk of disease. Results from a study in Hong Kong show that 90% of T2D patients are managed within the public healthcare system.
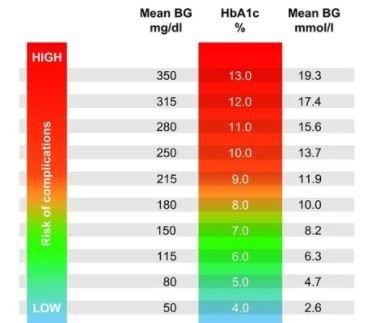
Researchers also found that a “moderate glycemic control goal” of between 6.5% and 7.5% was associated with lower dementia rates, but even lower glycemic targets were associated with an increased risk. I discovered that. The results were announced online on February 12, 2024. JAMA network open.
©Sophia Winters/stock.adobe.com
In a retrospective matched cohort study of more than 55,000 participants (mean age 62.3 years), researchers enrolled half of the group in a multidisciplinary primary care management program called the Risk Assessment and Management Program-Diabetes (RAMP-DM). program and the other half were randomly assigned. Half the usual care. During a median follow-up of 8.4 years, 6.97% of participants receiving RAMP-DM care received a diagnosis of dementia and 9.81% of participants receiving usual care received a diagnosis of dementia. I did. The dementia incidence rate per 1000 person-years was also lower in the RAMP-DM care group (9.31) than in the usual care group (14.02).
T2D is about 50% more likely to develop all-cause dementia, and Asians tend to be at higher risk, according to a study cited by lead author Kailu Wang, Ph.D., from the Chinese University of Hong Kong, and colleagues. Indeed, T2D is also associated with several pathological features of Alzheimer’s disease (AD), including vascular damage, hyperaccumulation of amyloid-β and tau phosphorylation, and chronic neuroinflammation. However, despite the known association, few studies have evaluated the effectiveness of glycemic control measures on dementia outcomes. Studies investigating intensive blood glucose lowering and the development of dementia have been limited by the use of surrogate endpoint markers and short follow-up periods.
Wang and his research team point to the success of the multidisciplinary RAMP-DM program established in Hong Kong in 2009 to enhance all aspects of T2D management and outcomes. In addition to hyperglycemia, RAMP-DM reduced the risk of death by 55%, macrovascular events by 48%, and microvascular events by 32% over a follow-up period of more than nine years, the researchers wrote. RAMP-DM is ideal for analyzing the effects of comprehensive T2D management services and their association with the risk of all-cause dementia and dementia subtypes, and for assessing the association between glycemic control and dementia development. provided a basic foundation.
To create the dataset for the retrospective study, Wang and colleagues intercepted the electronic medical records of every individual who used public health services in Hong Kong from 2011 to 2019. Researchers identified all adults diagnosed with T2D in 2011 (excluding those with type 1 diabetes). Gestational diabetes or pre-existing dementia. Researchers matched participants who received RAMP-DM plus usual care with patients who received usual care alone in a 1:1 ratio. Follow-up continued until the occurrence of an outcome event, death, or study end in December 2019.
The primary outcome was the incidence of dementia, and secondary outcomes included AD, VD, and other types of dementia. The primary analysis focused on RAMP-DM use and examined early HbA1C levels after RAMP-DM participation in relation to dementia incidence.
The number of participants in the final cohort after propensity score matching was 55,618. The mean age was 62.28 years, 51.4% were female, and participants were evenly divided into the RAMP-DM and usual care groups, 27,809 each. The overall mean time since T2D diagnosis was 5.9 years, and the mean baseline HbA1c level was 7.31%.
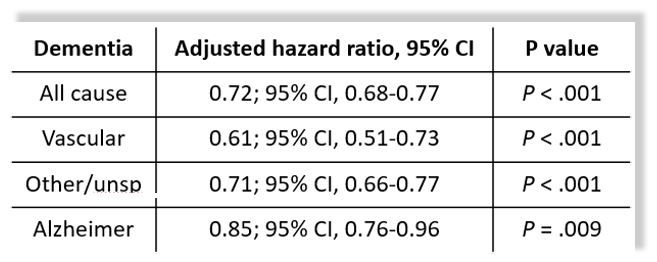
In addition to the reduced risk for all causes and subtypes of dementia associated with RAMP-DM use (table on the right), Wang et al. When examining the prevalence of dementia, HbA 1C levels ranged from 7.5% to 8.5% (aHR, 1.33; 95% CI, 1.19 to 1.48) and above were found to be at increased risk. <8.5% (aHR, 1.54; 95% CI, 1.31-1.80). Importantly, the researchers found that participants with lower HbA1C levels than the reference group, i.e., HbA1c 6% to 6.5% (aHR 1.17; 95% CI, 1.07 to 1.29, and HbA1C <6% (aHR)), They also found that the risk of dementia remains high among patients. , 1.39; 95% CI, 1.24-1.57).
“This cohort study of patients with T2D shows that a multidisciplinary and individualized diabetes management program in primary care settings is effective for patients with T2D in reducing the likelihood of all-cause dementia and its major subtypes. “We provided evidence that it is beneficial,” Wang et al. “Further studies may utilize prospective cohorts or RCTs to test the effectiveness of similar diabetes management interventions on dementia risk and investigate the biological mechanisms of such effects. “The cost-effectiveness of such programs to reduce the risk of cancer also requires further evaluation,” the researchers concluded.