Fraser A, Nelson SM, Macdonald-Wallis C, Cherry L, Butler E, Sattar N, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the avon longitudinal study of parents and children. Circulation. 2012;125(11):1367–80.
Google Scholar
Rich-Edwards JW, Fraser A, Lawlor DA, Catov JM. Pregnancy characteristics and women’s future cardiovascular health: an underused opportunity to improve women’s health? Epidemiol Rev. 2014;36(1):57–70.
Google Scholar
Sattar N, Greer IA. Pregnancy complications and maternal cardiovascular risk: opportunities for intervention and screening? BMJ. 2002;325(7356):157–60.
Google Scholar
Seely EW, Solomon CG. Insulin resistance and its potential role in pregnancy-induced hypertension. J Clin Endocrinol Metab. 2003;88(6):2393–8.
Google Scholar
Bosio PM, McKenna PJ, Conroy R, O’Herlihy C. Maternal central hemodynamics in hypertensive disorders of pregnancy. Obstet Gynecol. 1999;94(6):978–84.
Google Scholar
Redman CW, Sacks GP, Sargent IL. Preeclampsia: an excessive maternal inflammatory response to pregnancy. Am J Obstet Gynecol. 1999;180(2):499–506.
Google Scholar
Umesawa M, Kobashi G. Epidemiology of hypertensive disorders in pregnancy: prevalence, risk factors, predictors and prognosis. Hypertens Res. 2017;40(3):213–20.
Google Scholar
Obstetricians ACo, Gynecologists. Gestational hypertension and preeclampsia: ACOG Practice Bulletin, number 222. Obstet Gynecol. 2020;135(6):e237–60.
Behboudi-Gandevani S, Amiri M, Bidhendi Yarandi R, Ramezani TF. The impact of diagnostic criteria for gestational diabetes on its prevalence: a systematic review and meta-analysis. Diabetol Metab Syndr. 2019;11(1):1–18.
Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ (Clinical research ed). 2020;371:m3502.
Google Scholar
Wilkins-Haug L, Celi A, Thomas A, Frolkis J, Seely EW. Recognition by women’s health care providers of long-term cardiovascular disease risk after preeclampsia. Obstet Gynecol. 2015;125(6):1287–92.
Google Scholar
Young B, Hacker MR, Rana S. Physicians’ knowledge of future vascular disease in women with preeclampsia. Hypertens Pregnancy. 2012;31(1):50–8.
Google Scholar
Bellamy L, Casas J-P, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet (London, England). 2009;373(9677):1773–9.
Google Scholar
Giorgione V, Ridder A, Kalafat E, Khalil A, Thilaganathan B. Incidence of postpartum hypertension within 2 years of a pregnancy complicated by pre-eclampsia: a systematic review and meta-analysis. BJOG. 2021;128(3):495–503.
Google Scholar
Pathirana MM, Lassi Z, Ali A, Arstall M, Roberts CT, Andraweera PH. Cardiovascular risk factors in women with previous gestational diabetes mellitus: a systematic review and meta-analysis. Rev Endocr Metab Disord. 2021;22(4):729–61.
Google Scholar
Alonso-Ventura V, Li Y, Pasupuleti V, Roman YM, Hernandez AV, Perez-Lopez FR. Effects of preeclampsia and eclampsia on maternal metabolic and biochemical outcomes in later life: a systematic review and meta-analysis. Metabolism. 2020;102:154012.
Google Scholar
Bellamy L, Casas J-P, Hingorani AD, Williams DJ. Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335(7627):974.
Google Scholar
Bellou V, Belbasis L, Tzoulaki I, Evangelou E. Risk factors for type 2 diabetes mellitus: an exposure-wide umbrella review of meta-analyses. PLoS One. 2018;13(3):e0194127.
Google Scholar
Pittara T, Vyrides A, Lamnisos D, Giannakou K. Pre-eclampsia and long-term health outcomes for mother and infant: an umbrella review. BJOG. 2021;128(9):1421–30.
Google Scholar
Leslie MS, Briggs LA. Preeclampsia and the risk of future vascular disease and mortality: a review. J Midwifery Womens Health. 2016;61(3):315–24.
Google Scholar
Haas DM, Ehrenthal DB, Koch MA, Catov JM, Barnes SE, Facco F, et al. Pregnancy as a window to future cardiovascular health: design and implementation of the nuMoM2b heart health study. Am J Epidemiol. 2016;183(6):519–30.
Google Scholar
Adam S, McIntyre HD, Tsoi KY, Kapur A, Ma RC, Dias S, et al. Pregnancy as an opportunity to prevent type 2 diabetes mellitus: FIGO Best Practice Advice. Int J Gynecol Obstet. 2023;160:56–67.
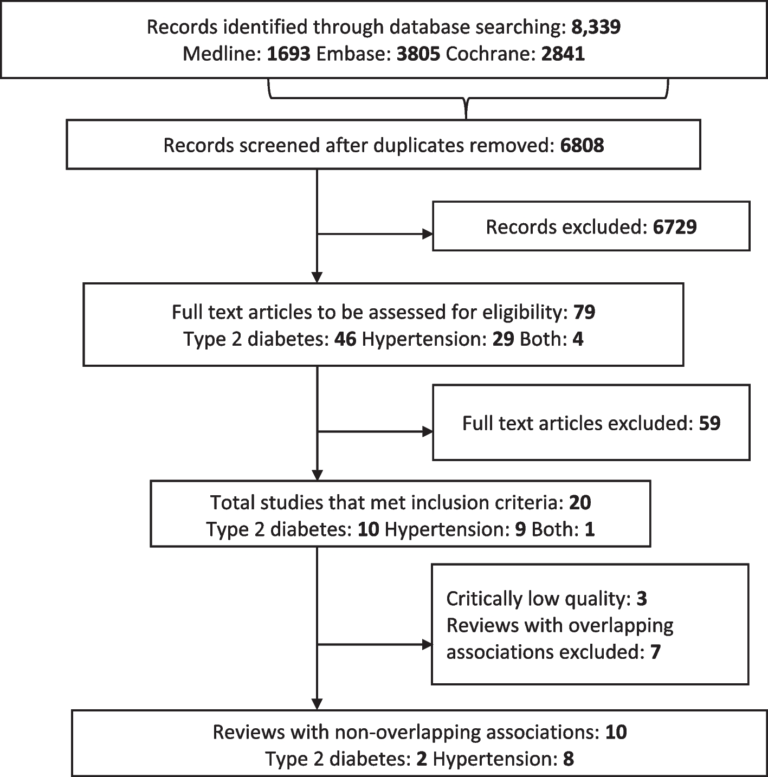
Moher D, Liberati A, Tetzlaff J, Altman DG, Group* P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Google Scholar
Singh M, Crowe F, Thangaratinam S, Abel KM, Black M, Okoth K, et al. Association of pregnancy complications/risk factors with the development of future long-term health conditions in women: overarching protocol for umbrella reviews. BMJ Open. 2022;12(12):e066476.
Google Scholar
MuM-PreDiCT Group. Multimorbidity in pregnancy: determinants, clusters, consequences and trajectories. Available from: https://mumpredict.org. Accessed 20 Feb 2023.
Lee E, Dobbins M, DeCorby K, McRae L, Tirilis D, Husson H. An optimal search filter for retrieving systematic reviews and meta-analyses. BMC Med Res Methodol. 2012;12(1):1–11.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Google Scholar
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Google Scholar
Hayden JA, van der Windt DA, Cartwright JL, Côté P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6.
Google Scholar
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute; 2000. Available from: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Smith V, Devane D, Begley CM, Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):1–6.
Pieper D, Antoine S-L, Mathes T, Neugebauer EA, Eikermann M. Systematic review finds overlapping reviews were not mentioned in every other overview. J Clin Epidemiol. 2014;67(4):368–75.
Google Scholar
Bougioukas KI, Liakos A, Tsapas A, Ntzani E, Haidich A-B. Preferred reporting items for overviews of systematic reviews including harms checklist: a pilot tool to be used for balanced reporting of benefits and harms. J Clin Epidemiol. 2018;93:9–24.
Google Scholar
Okoth K, Chandan JS, Marshall T, Thangaratinam S, Thomas GN, Nirantharakumar K, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review. BMJ. 2020;371:m3502.
Google Scholar
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. A decision tool to help researchers make decisions about including systematic reviews in overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):1–8.
Pollock M, Fernandes RM, Newton AS, Scott SD, Hartling L. The impact of different inclusion decisions on the comprehensiveness and complexity of overviews of reviews of healthcare interventions. Syst Rev. 2019;8(1):1–14.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. BMJ Ment Health. 2018;21(3):95–100.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Google Scholar
Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127(9):820–6.
Google Scholar
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Google Scholar
Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549.
Google Scholar
Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc A Stat Soc. 2009;172(1):137–59.
Google Scholar
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Google Scholar
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. Chichester: Wiley; 2019.
R Core Team. R: a language and environment for statistical computing; 2022. Available from: https://www.R-project.org/.
RStudio Team. RStudio: integrated development environment for R; 2022. Available from: http://www.rstudio.com/.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. BMJ Ment Health. 2019;22(4):153–60.
Bundhun PK, Soogund MZS, Huang F. Impact of systemic lupus erythematosus on maternal and fetal outcomes following pregnancy: a meta-analysis of studies published between years 2001–2016. J Autoimmun. 2017;79:17–27.
Google Scholar
Di Cianni G, Ghio A, Resi V, Volpe L. Gestational diabetes mellitus: an opportunity to prevent type 2 diabetes and cardiovascular disease in young women. Womens Health. 2010;6(1):97–105.
Edstedt Bonamy AK, Parikh NI. Predicting women’s future cardiovascular health from pregnancy complications. Curr Cardiovasc Risk Rep. 2013;7(3):173–82.
Gortner L. Intrauterine growth restriction and risk for arterial hypertension: a causal relationship? J Perinat Med. 2007;35(5):361–5.
Google Scholar
Guo J, Chen J-L, Whittemore R, Whitaker E. Postpartum lifestyle interventions to prevent type 2 diabetes among women with history of gestational diabetes: a systematic review of randomized clinical trials. J Womens Health (2002). 2016;25(1):38–49.
Hutchesson M, Campbell L, Leonard A, Vincze L, Shrewsbury V, Collins C, et al. Do modifiable risk factors for cardiovascular disease post-pregnancy influence the association between hypertensive disorders of pregnancy and cardiovascular health outcomes? A systematic review of observational studies. Pregnancy Hypertens. 2022;27:138–47.
Google Scholar
Jenabi E, Afshari M, Khazaei S. The association between preeclampsia and the risk of metabolic syndrome after delivery: a meta-analysis. J Matern Fetal Neonatal Med. 2021;34(19):3253–8.
Google Scholar
Kramer CK, Campbell S, Retnakaran R. Gestational diabetes and the risk of cardiovascular disease in women: a systematic review and meta-analysis. Diabetologia. 2019;62(6):905–14.
Google Scholar
Lao TT. The mother – the long-term implications on metabolic and cardiovascular complications. Best Pract Res Clin Obstet Gynaecol. 2015;29(2):244–55.
Google Scholar
Lassi ZS, Bhutta ZA. Risk factors and interventions related to maternal and pre-pregnancy obesity, pre-diabetes and diabetes for maternal, fetal and neonatal outcomes: a systematic review. Expert Rev Obstet Gynecol. 2013;8(6):639–60.
Google Scholar
Leya M, Armstrong LL, Scheftner DA, Lowe WL, Hayes MG, Lowe LP, et al. Association of plasma glucose and type 2 diabetes susceptibility genes with gestational diabetes. Diabetes. 2013;62(SUPPL. 1):A431.
Li M, Rawal S, Hinkle S, Liu S, Tekolaayele F, Zhang C. Sex hormone-binding globulin, cardiometabolic biomarkers, and gestational diabetes-a longitudinal pregnancy cohort study and a meta-analysis. Diabetes. 2018;67(Supplement 1):A384–5.
Li P, Shan Z, Zhou L, Xie M, Bao W, Zhang Y, et al. Parity and risk of type 2 diabetes: a systematic review and dose-response meta-analysis. Eur J Endocrinol. 2016;175(5):R231–45.
Google Scholar
Li S, Xi B. Preterm birth is associated with risk of essential hypertension in later life. Int J Cardiol. 2014;172(2):e361–3.
Google Scholar
Li W, Ruan W, Lu Z, Wang D. Parity and risk of maternal cardiovascular disease: a dose-response meta-analysis of cohort studies. Eur J Prev Cardiol. 2019;26(6):592–602.
Google Scholar
Liao L, Deng Y, Zhao D. Association of low birth weight and premature birth with the risk of metabolic syndrome: a meta-analysis. Front Pediatr. 2020;8:405.
Google Scholar
Lin Z, Wang Y, Zhang B, Jin Z. Association of type 2 diabetes susceptible genes GCKR, SLC30A8, and FTO polymorphisms with gestational diabetes mellitus risk: a meta-analysis. Endocrine. 2018;62(1):34–45.
Google Scholar
Liu J, Song G, Zhao G, Meng T. Lack of association between IGF2BP2 rs4402960 polymorphism and gestational diabetes mellitus: a case-control study, meta-analysis and trial sequential analysis. Biosci Rep. 2020;40(7):BSR20200990.
Google Scholar
Mao H, Li Q, Gao S. Meta-analysis of the relationship between common type 2 diabetes risk gene variants with gestational diabetes mellitus. PLoS One. 2012;7(9):e45882.
Google Scholar
McIntyre HD, Kapur A, Divakar H, Hod M. Gestational diabetes mellitus-innovative approach to prediction, diagnosis, management, and prevention of future NCD-mother and offspring. Front Endocrinol. 2020;11:614533.
Minhas AS, Ying W, Ogunwole SM, Miller M, Zakaria S, Vaught AJ, et al. The association of adverse pregnancy outcomes and cardiovascular disease: current knowledge and future directions. Curr Treat Options Cardiovasc Med. 2020;22(12):61.
Google Scholar
Moore LE, Voaklander B, Savu A, Yeung RO, Ryan E, Chojecki D, et al. Association between the antepartum oral glucose tolerance test and the risk of future diabetes mellitus among women with gestational diabetes: a systematic review and meta-analysis. J Diabetes Complications. 2021;35(4):107804.
Google Scholar
Morton S, Kirkwood S, Thangaratinam S. Interventions to modify the progression to type 2 diabetes mellitus in women with gestational diabetes: a systematic review of literature. Curr Opin Obstet Gynecol. 2014;26(6):476–86.
Google Scholar
Neiger R. Long-term effects of pregnancy complications on maternal health: a review. J Clin Med. 2017;6(8):76.
Google Scholar
Noctor E. Risk associated with development of type 2 DM in gestational diabetes. Clin Chem Lab Med. 2019;57(8):eA105.
Park K, Minissian MB, Wei J, Saade GR, Smith GN. Contemporary clinical updates on the prevention of future cardiovascular disease in women who experience adverse pregnancy outcomes. Clin Cardiol. 2020;43(6):553–9.
Google Scholar
Peacock AS, Bogossian F, McIntyre HD, Wilkinson S. A review of interventions to prevent type 2 diabetes after gestational diabetes. Women Birth. 2014;27(4):e7–15.
Google Scholar
Pedersen ALW, Terkildsen Maindal H, Juul L. How to prevent type 2 diabetes in women with previous gestational diabetes? A systematic review of behavioural interventions. Prim Care Diabetes. 2017;11(5):403–13.
Google Scholar
Pons MB, Badia OA. A systematic review with meta analysis of women with gestational diabetes indicate that they are at risk to suffer diabetes seven times more than normoglycemic women: commentary. FMC Form Med Contin Atencion Prim. 2010;17(3):200.
Reddy M, Palmer K, Rolnik D, Mol B, Wallace E, Costa F. Preeclampsia and long-term cardiovascular function – a systematic review and meta-analysis. J Paediatr Child Health. 2019;55(Supplement 1):96.
Sangtani A, Alrahmani L, Parikh P. Effect of hypertensive disorders of pregnancy on clinical outcomes in peripartum cardiomyopathy. Obstet Gynecol. 2019;133(SUPPL 1):105S.
Steinthorsdottir V, McGinnis R, Williams NO, Stefansdottir L, Thorleifsson G, Shooter S, et al. Genetic predisposition to hypertension is associated with preeclampsia in European and Central Asian women. Nat Commun. 2020;11(1):5976.
Google Scholar
Tranidou A, Dagklis T, Tsakiridis I, Siargkas A, Apostolopoulou A, Mamopoulos A, et al. Prevalence of metabolic syndrome after pregnancies complicated by gestational diabetes mellitus – a systematic review and meta-analysis. Clin Nutr ESPEN. 2020;40:539–40.
Tranidou A, Dagklis T, Tsakiridis I, Siargkas A, Apostolopoulou A, Mamopoulos A, et al. Risk of developing metabolic syndrome after gestational diabetes mellitus – a systematic review and meta-analysis. J Endocrinol Invest. 2021;44(6):1139–49.
Google Scholar
Varner MW, Rice MM, Landon MB, Casey BM, Reddy UM, Wapner RJ, et al. Pregnancies after the diagnosis of mild gestational diabetes mellitus and risk of cardiometabolic disorders. Obstet Gynecol. 2017;129(2):273–80.
Google Scholar
Visser S, Hermes W, Ket JCF, Otten RHJ, van Pampus MG, Bloemenkamp KWM, et al. Systematic review and metaanalysis on nonclassic cardiovascular biomarkers after hypertensive pregnancy disorders. Am J Obstet Gynecol. 2014;211(4):373.e1-9.
Google Scholar
Wang Z, Kanguru L, Hussein J, Fitzmaurice A, Ritchie K. Incidence of adverse outcomes associated with gestational diabetes mellitus in low- and middle-income countries. Int J Gynecol Obstet. 2013;121(1):14–9.
Lo CCW, Lo ACQ, Leow SH, Fisher G, Corker B, Batho O, et al. Future cardiovascular disease risk for women with gestational hypertension: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(13):e013991.
Google Scholar
Xu Y, Shen S, Sun L, Yang H, Jin B, Cao X. Metabolic syndrome risk after gestational diabetes: a systematic review and meta-analysis. PLoS One. 2014;9(1):e87863.
Google Scholar
Zhao G, Bhatia D, Jung F, Lipscombe L. 47 – risk of type 2 diabetes mellitus after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Can J Diabetes. 2020;44(7 Supplement):S21.
Baptiste-Roberts K, Barone BB, Gary TL, Golden SH, Wilson LM, Bass EB, et al. Risk factors for type 2 diabetes among women with gestational diabetes: a systematic review. Am J Med. 2009;122(3):207-14.e4.
Google Scholar
Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes mellitus and its association with type 2 diabetes. Diabet Med. 2004;21(2):103–13.
Google Scholar
Burger RJ, Delagrange H, van Valkengoed IGM, de Groot CJM, van den Born BJH, Gordijn SJ, et al. Hypertensive disorders of pregnancy and cardiovascular disease risk across races and ethnicities: a review. Front Cardiovasc Med. 2022;9:933822.
Google Scholar
Cao S, Li N, Zhang C, Liu J, Wang H, Leng J, et al. Adverse pregnancy outcomes are associated with an increased risk of postpartum prediabetes and diabetes in Chinese women with gestational diabetes. Diabetes Res Clin Pract. 2022;186:109817.
Google Scholar
Craici IM, Wagner SJ, Hayman SR, Garovic VD. Pre-eclamptic pregnancies: an opportunity to identify women at risk for future cardiovascular disease. Womens Health (Lond). 2008;4(2):133–5.
Google Scholar
Farahvar S, Walfisch A, Sheiner E. Gestational diabetes risk factors and long-term consequences for both mother and offspring: a literature review. Expert Rev Endocrinol Metab. 2019;14(1):63–74.
Google Scholar
Groenhof TKJ, van Rijn BB, Franx A, Roeters van Lennep JE, Bots ML, Lely AT. Preventing cardiovascular disease after hypertensive disorders of pregnancy: Searching for the how and when. Eur J Prev Cardiol. 2017;24(16):1735–45.
Google Scholar
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–8.
Google Scholar
Krome S. Gestational diabetes: individual risk assessment for type 2 diabetes. Diabetol Stoffwechsel. 2016;11(4):248–50.
Rayanagoudar G, Hashi AA, Zamora J, Khan KS, Hitman GA, Thangaratinam S. Quantification of the type 2 diabetes risk in women with gestational diabetes: a systematic review and meta-analysis of 95,750 women. Diabetologia. 2016;59(7):1403–11.
Google Scholar
Ganesh A, Sarna N, Mehta R, Smith E. Hypertensive disorders in pregnancy and future risk of stroke: a systematic review (P2. 114). Minneapolis: AAN Enterprises; 2014.
Veiga ECDA, Rocha PRH, Caviola LL, Cardoso VC, Costa FDS, Saraiva MDCP, et al. Previous preeclampsia and its association with the future development of cardiovascular diseases: a systematic review and meta-analysis. Clinics. 2021;76:e1999.
Google Scholar
Wu P, Haththotuwa R, Kwok CS, Babu A, Kotronias RA, Rushton C, et al. Preeclampsia and future cardiovascular health: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2017;10(2):e003497.
Google Scholar
Brouwers L, van der Meiden-van Roest AJ, Savelkoul C, Vogelvang TE, Lely AT, Franx A, et al. Recurrence of pre-eclampsia and the risk of future hypertension and cardiovascular disease: a systematic review and meta-analysis. BJOG. 2018;125(13):1642–54.
Google Scholar
Dennison RA, Chen ES, Green ME, Legard C, Kotecha D, Farmer G, et al. The absolute and relative risk of type 2 diabetes after gestational diabetes: a systematic review and meta-analysis of 129 studies. Diabetes Res Clin Pract. 2021;171:108625.
Google Scholar
Li Z, Cheng Y, Wang D, Chen H, Chen H, Ming W-K, et al. Incidence rate of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review and meta-analysis of 170,139 women. J Diabetes Res. 2020;2020:3076463.
Google Scholar
Song C, Lyu Y, Li C, Liu P, Li J, Ma RC, et al. Long-term risk of diabetes in women at varying durations after gestational diabetes: a systematic review and meta-analysis with more than 2 million women. Obes Rev. 2018;19(3):421–9.
Google Scholar
Wang Z, Wang Z, Wang L, Qiu M, Wang Y, Hou X, et al. Hypertensive disorders during pregnancy and risk of type 2 diabetes in later life: a systematic review and meta-analysis. Endocrine. 2017;55(3):809–21.
Google Scholar
Wu P, Kwok CS, Haththotuwa R, Kotronias RA, Babu A, Fryer AA, et al. Pre-eclampsia is associated with a twofold increase in diabetes: a systematic review and meta-analysis. Diabetologia. 2016;59(12):2518–26.
Google Scholar
You H, Hu J, Liu Y, Luo B, Lei A. Risk of type 2 diabetes mellitus after gestational diabetes mellitus: a systematic review & meta-analysis. Indian J Med Res. 2021;154(1):62–77.
Google Scholar
Hopmans TEJP, Van Houten CB, Kasius A, Kouznetsova OI, Nguyen AL, Rooijmans SV, et al. Increased risk of type 2 diabetes mellitus and cardiovascular disease after diabetes gravidarum. Ned Tijdschr Geneeskd. 2015;159(24):A8043.
Google Scholar
Cavalli R, Veiga E, Rocha P, Cardoso V, Bettiol H. P-099. Previous preeclampsia and its association with future cardiovascular diseases: a systematic review and meta-analysis. Pregnancy Hypertens. 2021;25(1):e61.
Wu R, Wang T, Gu R, Xing D, Ye C, Chen Y, et al. Hypertensive disorders of pregnancy and risk of cardiovascular disease-related morbidity and mortality: a systematic review and meta-analysis. Cardiology. 2020;145(10):633–47.
Google Scholar
Gadve SS, Chavanda S, Mukherjee AD, Aziz S, Joshi A, Patwardhan M. Risk of developing type 2 diabetes mellitus in south asian women with history of gestational diabetes mellitus: a systematic review and meta-analysis. Indian J Endocrinol Metab. 2021;25(3):176–81.
Google Scholar
Xu J, Li T, Wang Y, Xue L, Miao Z, Long W, et al. The association between hypertensive disorders in pregnancy and the risk of developing chronic hypertension. Front Cardiovasc Med. 2022;9:897771.
Google Scholar
Sukmanee J, Liabsuetrakul T. Risk of future cardiovascular diseases in different years postpartum after hypertensive disorders of pregnancy: a systematic review and meta-analysis. Medicine. 2022;101(30):e29646.
Google Scholar
Vounzoulaki E, Khunti K, Abner SC, Tan BK, Davies MJ, Gillies CL. Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ. 2020;369:m1361.
Google Scholar
Zhao G, Bhatia D, Jung F, Lipscombe L. Risk of type 2 diabetes mellitus in women with prior hypertensive disorders of pregnancy: a systematic review and meta-analysis. Diabetologia. 2021;64(3):491–503.
Google Scholar
Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R. Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28(1):1–19.
Google Scholar
Dall’Asta A, D’Antonio F, Saccone G, Buca D, Mastantuoni E, Liberati M, et al. Cardiovascular events following pregnancy complicated by pre-eclampsia with emphasis on comparison between early- and late-onset forms: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2021;57(5):698–709.
Google Scholar
Groenhof TKJ, Zoet GA, Franx A, Gansevoort RT, Bots ML, Groen H, et al. Trajectory of cardiovascular risk factors after hypertensive disorders of pregnancy: an argument for follow-up. Hypertension. 2019;73(1):171–8.
Google Scholar
Berks D, Steegers EA, Molas M, Visser W. Resolution of hypertension and proteinuria after preeclampsia. Obstet Gynecol. 2009;114(6):1307–14.
Google Scholar
Sibai BM. Etiology and management of postpartum hypertension-preeclampsia. Am J Obstet Gynecol. 2012;206(6):470–5.
Google Scholar
Cornell JE, Mulrow CD, Localio R, Stack CB, Meibohm AR, Guallar E, et al. Random-effects meta-analysis of inconsistent effects: a time for change. Ann Intern Med. 2014;160(4):267–70.
Google Scholar
Bender R, Friede T, Koch A, Kuss O, Schlattmann P, Schwarzer G, et al. Methods for evidence synthesis in the case of very few studies. Res Synth Methods. 2018;9(3):382–92.
Google Scholar
Riley RD, Debray TP, Fisher D, Hattle M, Marlin N, Hoogland J, et al. Individual participant data meta-analysis to examine interactions between treatment effect and participant-level covariates: statistical recommendations for conduct and planning. Stat Med. 2020;39(15):2115–37.
Google Scholar
Zhang C, Bao W, Rong Y, Yang H, Bowers K, Yeung E, et al. Genetic variants and the risk of gestational diabetes mellitus: a systematic review. Hum Reprod Update. 2013;19(4):376–90.
Google Scholar
Semenkovich CF. Insulin resistance and atherosclerosis. J Clin Investig. 2006;116(7):1813–22.
Google Scholar
Ruksasakul R, Tharavanij T, Sritipsukho P. Metabolic syndrome in thai women previously diagnosed with gestational diabetes. J Med Assoc Thailand. 2016;99:S195-202.
Alageel S, Wright AJ, Gulliford MC. Changes in cardiovascular disease risk and behavioural risk factors before the introduction of a health check programme in England. Prev Med. 2016;91:158–63.
Google Scholar
The National Institute for Health and Care Excellence (NICE). Hypertension in pregnancy: diagnosis and management; 2019. (NICE guideline [NG133]).
The National Institute for Health and Care Excellence (NICE). Type 2 diabetes: prevention in people at high risk; 2017.
Hippisley-Cox J, Coupland C. Development and validation of QDiabetes-2018 risk prediction algorithm to estimate future risk of type 2 diabetes: cohort study. BMJ. 2017;359:j5019.
Google Scholar
Parikh NI, Pencina MJ, Wang TJ, Benjamin EJ, Lanier KJ, Levy D, et al. A risk score for predicting near-term incidence of hypertension: the Framingham Heart Study. Ann Intern Med. 2008;148(2):102–10.
Google Scholar