In a world where the pursuit of longevity faces the challenges of aging, two recent studies shed light on the complex dance between physical health and cognitive function during the golden years. One study focuses on the quiet cries of the spine and whispers of cognitive decline, while another reveals the double-edged sword of antibiotics and how they affect our attempts to fight disease and how it affects us. It paints a complex picture of unintended consequences for the mind.
The Story of the Spine: A Story of Pain and Memory
Imagine your spine as a hierarchical pillar that holds the secrets to not only your physical but also your cognitive health. A groundbreaking study reveals a surprising correlation between spinal pain and cognitive function in older adults, highlighting a gender-specific relationship. Older men who suffer from both back and neck pain were found to have lower cognitive scores than women. The findings point out that spinal pain is not just a physical illness, but also a modifiable risk factor for cognitive decline, and that neurodegenerative pathways have implications for what we see as just a sign of aging. This suggests that there may be a lot of pain that we tend to ignore.
The antibiotic paradox: the body heals, but the mind hurts
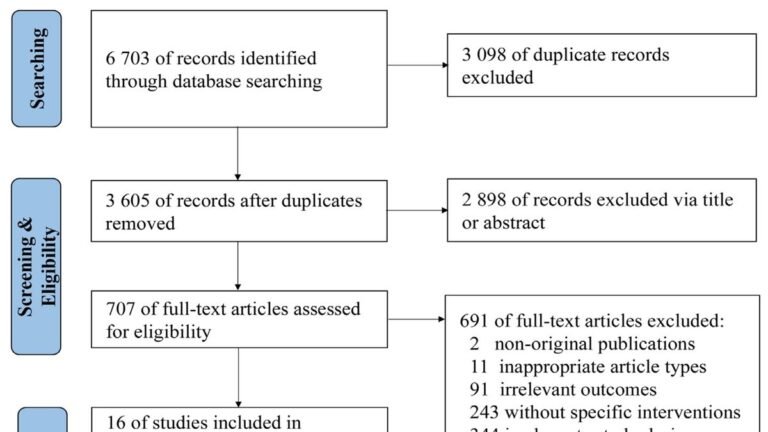
In an era when antibiotics have become reliable warriors in the fight against infectious diseases, their long-term effects on cognition unfold a story with unexpected consequences. A systematic review and meta-analysis of 17 studies reveals the dark side of our fight against microbes. Long-term or repeated antibiotic use appears to have a significant effect on chronic cognitive performance, impairing cognitive performance at any age. This effect has been noted prominently in pediatric studies, highlighting the critical developmental stage where the effects of antibiotics on cognition may be most profound.
Among the clinical trials analyzed, there was a glimmer of hope for doxycycline and rifampicin to improve cognitive outcomes in patients with mild to moderate Alzheimer’s disease. However, this silver lining was clouded by the results of a large study showing that the same treatment resulted in significant cognitive decline compared to a placebo, leading to a loss of effectiveness of known cognitive enhancers, cholinesterase inhibitors. It suggests possibility. These discoveries illuminate the complex interactions between disease, treatment, and cognitive health and help us navigate the murky waters of pharmaceutical interventions.
Uncovering the complex relationship between health and cognition
These studies serve as important guideposts as we stand at a crossroads in advancing medicine and understanding human health holistically. These not only call into question our approaches to treating physical illnesses, but also call for deeper investigation into how these treatments resonate in the corridors of cognitive health. Efforts to understand and reduce cognitive decline in older adults are proving to require not only reevaluating treatment strategies but also looking beyond traditional risk factors. In this delicate balance of health and disease, the double-edged sword of spinal resilience and antibiotics emerges as important pieces of the puzzle in maintaining cognitive function as we age.
In conclusion, the intersection of spine health and antibiotic use with cognitive function opens new avenues for research and intervention strategies. The quest to maintain cognitive health as we navigate the complexities of aging requires a holistic approach that considers the multifaceted interactions between physical health, medical treatments, and cognitive outcomes. These findings highlight the importance of adjusting medical practice not only to address symptoms but also to protect the cognitive health of aging populations, ensuring that the journey to golden years is not limited to longevity alone. guarantees that it is characterized by the maintenance of quality of life.