The research Proceedings of the National Academy of Sciences (PNAS) We show how the presence of a specific protein called IL-22BP affects the composition of the gut microbiota and the body’s response to bacterial infection.
“We found that mice that did not produce this protein were more protected against intestinal infections caused by bacteria such as: Clostridioides difficile and Citrobacter rodentium“This is a new finding,” said study co-author Marco Aurélio Ramirez Vinoro, a professor at the Institute of Biology at the State University of Campinas (IB-UNICAMP) in Brazil and head of the institute’s Laboratory of Immuno-Inflammation.
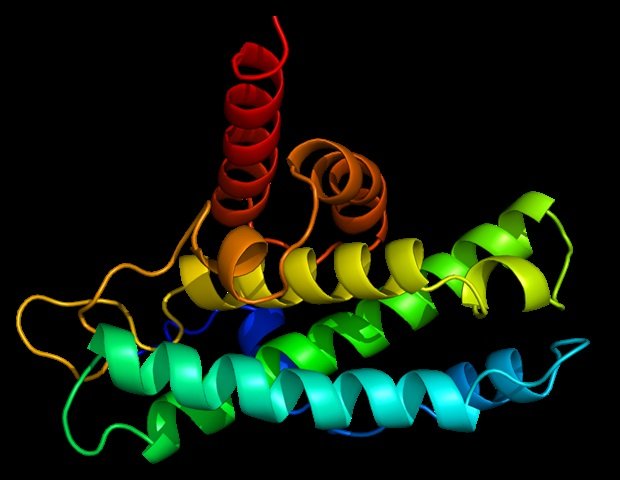
IL-22BP (interleukin-22 binding protein) reduces the available amount of IL-22, a protein produced by immune system cells that is involved in maintaining the intestinal barrier, strengthening gut lining cells, and producing antibacterial substances.
“Our explanation for this finding is that interleukin-22 is more effective in the absence of IL-22BP in strengthening the intestinal defense even before the infection begins,” said Vignolo, who received funding from FAPESP to study molecular mechanisms involved in the gut microbiota during inflammation.
In the PNAS article, the researchers report that mice lacking IL-22BP had different gut bacteria, and when they transferred these bacteria to mice with normal production of IL-22BP, the mice were protected from infection, suggesting that the lack of the binding protein resulted in beneficial modulation of the gut microbiota.
“This infection resistance is associated with increased production of short-chain fatty acids, which are released through the fermentation of dietary fibre by gut bacteria and have beneficial effects on gut health, such as promoting an anti-inflammatory environment and strengthening the intestinal barrier,” said lead author José Luis Fati, a postdoctoral researcher at Washington University School of Medicine (WUSM) in the US.
Fati was supported by FAPESP during his doctoral research on gut microbiota-colonization interactions. it’s difficultis a bacillus that is resistant to some antibacterial agents and is a frequent cause of hospital-acquired infections. Short-chain fatty acids are produced by bacterial metabolism during the fermentation of dietary fiber and protect the intestine from infection. it’s difficult.
According to Vinoro, Dr. Fati’s thesis supervisor, the lack of IL-22BP alters the composition and function of the gut microbiota, resulting in a beneficial microbial profile. “This highlights the role of the gut microbiota in modulating microbial responses and suggests that IL-22BP inhibition may be able to attenuate or prevent intestinal infections,” he said.
Next steps
Future studies can be designed to better understand this finding and help develop treatments. “An important next step is to examine the efficacy of IL-22BP inhibitors in animal models and conduct clinical trials to treat severe intestinal infections,” Fati said. Another possibility is to examine how the type and amount of dietary fiber affects the production of short-chain fatty acids. “The composition of the gut microbiota in the absence of IL-22BP could provide valuable information,” he added.
Modulation of the gut microbiota may also have benefits in other intestinal inflammatory diseases, such as Crohn’s disease and ulcerative colitis, as well as infections caused by other pathogens.
“Knowing how IL-22 interacts with other molecules and immune system cells in the absence of IL-22BP will help us to better understand its function in intestinal immunity. Future studies may change our understanding of the role of these proteins in intestinal health and lead to the development of new therapeutic strategies to prevent and treat intestinal infections,” said Vignolo.
The study involved researchers from the Department of Genetics, Evolution, Microbiology and Immunology at IB-UNICAMP and the Department of Pathology and Immunology at WUSM.
sauce:
Sao Paulo Research Foundation (FAPESP)
Journal References:
Fati, J.L. other. (2024). Deficiency of IL-22-binding protein enhances the gut microbiota’s defense against enteric pathogens. Proceedings of the National Academy of Sciences. doi.org/10.1073/pnas.2321836121.