[Originally published: Dec. 7, 2022. Updated: Oct. 20, 2023]
In 2022, the Food and Drug Administration (FDA) approved a drug that delays the onset of type 1 diabetes. This is the first treatment to change the course of this autoimmune disease since the discovery of insulin in 1922.
The drug, called teplizumab and sold under the brand name Tzield®, is intended for patients with stage 2 type 1 diabetes (aged 8 years and older), who researchers say are newly diagnosed with the disease. We continue to research ways to further help children and young people. .
To this end, a paper was published in mid-October. New England Medical Journal (NEJM) Two 12-day courses of teplizumab in children and adolescents diagnosed with diabetes within the past six weeks preserved their ability to make their own insulin, a promising study found.
In type 1 diabetes, the beta cells of the pancreas produce little or no insulin. Insulin is a hormone needed to help glucose (blood sugar) get into the body’s cells so it can be used for energy. Without insulin, blood sugar builds up in the bloodstream, causing a variety of symptoms.
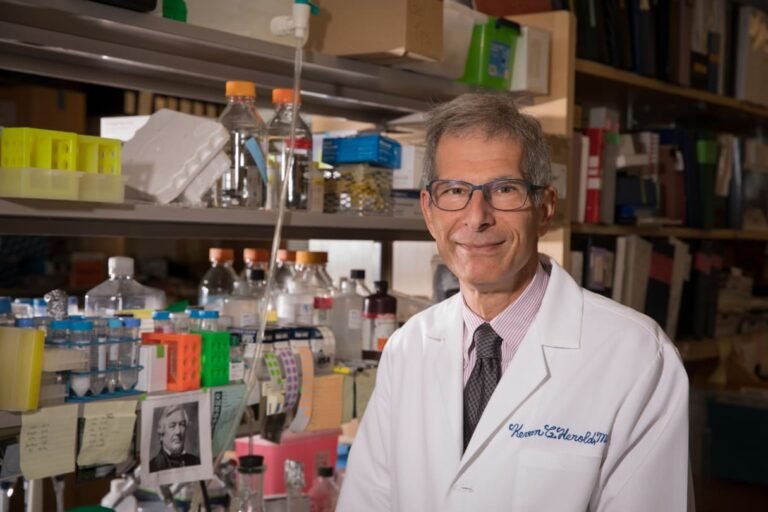
Type 1 diabetes has different stages. In stage 1, blood sugar levels are normal, but autoantibodies to insulin-producing beta cells (a marker of disease activity) begin to appear in the bloodstream, causing the beta cells to die, preparing to progress to stages 2 and 3. is in place. Kevan Herold, M.D., an endocrinologist at Yale University who participated in the teplizumab trial and is an author of the latest paper, explains. NEJM Research (called PROTECT).
“In stage 2, the attack on the beta cells is ongoing, but blood sugar levels are still normal unless certain types of tests, such as glucose tolerance tests, identify an impaired beta cell response,” says Dr. Herold. Masu. “The risk of developing stage 3, or clinical diabetes, within two years is about 50%.”
The goal of teplizumab is to delay as much as possible the onset of clinical diabetes, with typical symptoms such as excessive urination, thirst, and other complications. Researchers say the drug delays the onset of the disease by a median of at least two years.
Most people who develop type 1 diabetes have no relatives with the disease and may not know that they are at risk of being diagnosed with type 1 diabetes. “Thus, most patients present to the doctor’s office or emergency room with stage 3 type 1 diabetes, where they experience typical symptoms of the disease, including diabetic ketoacidosis, a serious diabetes-related complication. It’s already showing up,” Dr. Herold added.
The PROTECT trial administered teplizumab to children and adolescents with stage 3 type 1 diabetes to test whether the drug prevented the destruction of beta cell function even after diagnosis.
“This drug helps people maintain their ability to make their own insulin. We know that children, especially those who first develop diabetes, lose that ability over many years,” Herold said. says the doctor. “This won’t stop it completely, but it will slow down the process and buy the pancreas time to work. This is because the human pancreas is always better at delivering insulin than using artificial means. It is very helpful for children and adults who are new to diabetes.”
Below, Dr. Herold answers more questions about the future of pharmacotherapy and diabetes management.