CLINICAL RELEVANCE: Maternal mortality rates in the United States have skyrocketed in recent years, reaching 32.9 deaths per 100,000 live births in 2021.
- Black women have a significantly higher maternal mortality rate of 69.9 per 100,000 live births, highlighting racial disparities.
- Research suggests that mental illness contributes significantly to maternal mortality, with almost one in four deaths linked to a mental health disorder.
- To effectively address the maternal health crisis, policy changes such as increased mental health screening of mothers and paid parental leave have been advocated.
Even though progress has changed childbirth Maternal mortality rates in the United States are gradually increasing due to (mostly) routine procedures.
In 2021, the U.S. maternal mortality rate was 32.9 deaths per 100,000 live births. This is an alarming rise from 23.8 in 2020 and 20.1 in 2019, according to the latest data. Centers for Disease Control and Prevention.
That’s tragic enough. However, the maternal mortality rate for black women jumped to 69.9 deaths per 100,000 live births. This is 2.6 times the rate for non-Hispanic white women (26.6).
but why?
A research team led by National Children’s Hospital wanted to find out why. So the group combed through years of data. They found that mental illness may be behind the alarming rise in mortality rates. The group examined 30 peer-reviewed studies and more than a dozen health policy publications.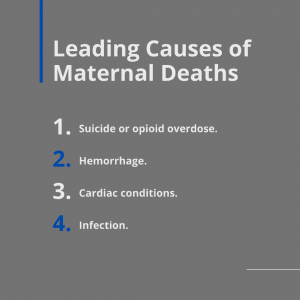
JAMA Psychiatry This result was announced the study In the latest version.
“The contribution of mental health conditions to the maternal morbidity and mortality crisis in the United States is not widely recognized,” study co-author Katherine L. Wisner, MD, explained in the paper. press release. “We need to bring this to the attention of the public and policymakers and demand action to address the mental health crisis that contributes to the deaths of American mothers.”
Shocking maternal mortality statistics
Reviews painted a disturbing picture.
- Health care professionals can prevent more than 80% of maternal deaths in the United States.
- Researchers have directly linked almost one in four maternal deaths to mental health disorders.
- Overdoses, like other maternal mental health conditions, kill more than twice as many women as postpartum hemorrhage, the second leading cause of maternal death.
Worse, despite federal and state investments to stem the tide of maternal deaths, including more than $100 million in state programs to improve maternal health care access, However, researchers have found that it is failing to contain the “public health crisis it represents.” ”
Other highlights of the research review include:
- Studies show that during the perinatal period, women are at increased risk for mental illness. More than 14% of pregnant mothers admit the development of new diseases. depression. An additional 14.5% develop an episode within the first 90 days of life.
- From 2006 to 2020, more than 400 maternity medical centers closed across the United States. This has created what researchers call an “obstetric care desert,” leaving nearly 6 million women with limited or no access to obstetric care.
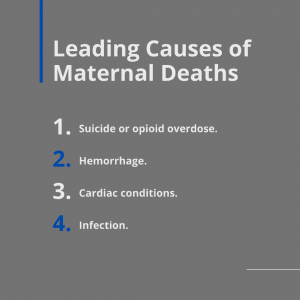
- Mental health conditions, including suicide and opioid overdose, account for nearly 23% of maternal deaths. This was followed by bleeding (13.7%), heart disease (12.8%), and infection (9.2%).
Researchers drive new priorities
Wisner, associate director of perinatal mental health and a member of Children’s National’s Center for Prenatal, Postnatal, Newborn, and Maternal Health Research, said she believes health care professionals screen new mothers for postpartum depression. only about 20 percent, he added.
“Given that this is a time when many mothers come into contact with health professionals, it is critical that all mothers are tested and offered treatment,” she said. “Mental health is fundamental to the health of mothers, children and the entire family.”
Researchers say policymakers need to consider a fundamental shift in the way they approach maternal health. For example, the authors call for at least two to three months of paid parental leave.
“Rather than focusing on a relatively small number of contributors to health, which current medical practice targets, by strengthening the social foundations we can improve the future health of families through culturally appropriate, patient-centered care.” “The outlook for the future is strengthened,” the study authors concluded. “It’s past time to embrace this shift in thinking about health holistically. Mental health is the foundation of wellness.”
References
Prevalence and correlates of perinatal self-harm
Treatment of comorbid perinatal depression and PTSD in socio-economically disadvantaged women.
Childhood trauma and perinatal depression


