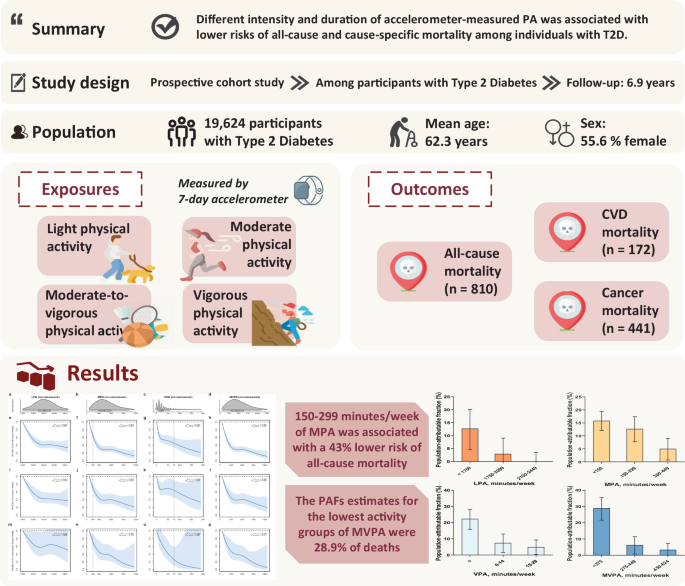
Study design and participants
The datasets used in this study were obtained from the UK Biobank (application number: 79095) and approved by the Northwest Multicentre Research Ethics Committee (R21/NW/0157) and the Biomedical Research Ethics Committee of Hangzhou Normal University (200400001). All participants gave written informed consent and signed an informed consent form agreeing to linking to the National Electronic Health-related Datasets.32The UK Biobank is a large population-based prospective cohort in which over 500,000 participants aged 37–73 years visited one of 22 assessment centres in England, Scotland and Wales between 2006 and 2010 (UK Biobank baseline) to complete a touchscreen questionnaire, physical examination and biological sample collection. 240,000 invitations were then sent randomly for physical activity measurement by accelerometer between 2013 and 2015 (baseline for the main study), with a response rate of 44%. Devices were sent out to 106,053 participants, of whom data were received from 103,666. In the main study, participants with type 2 diabetes at baseline were included if they had self-reported type 2 diabetes, randomly measured blood glucose ≥11.1 mmol/L, or glycated hemoglobin (HbA1c) levels ≥48 mmol/L according to the American Diabetes Association criteria and code E11 in the electronic health record (England and Wales: Health Episode Statistics; Scotland: Scottish Disease Register) according to the International Classification of Diseases, 10th Revision (ICD-10). The algorithm for capture and adjudication of prevalent T2D was consistent with previous studies.9.
Physical activity measured by device
Participants were asked to wear an Axivity AX3 (Newcastle upon Tyne, UK) triaxial accelerometer on their dominant hand for 7 days, with the sensor capturing 100 Hz acceleration with a dynamic range of ±8 g (gravity units).13Participants with insufficient wear time (<72 h), insufficient device calibration, or who experienced a daylight saving time change during the wear period were excluded from the study. Minutes per week of LPA, MPA, and VPA were determined as time spent in activities with an intensity of 30–125 milligravity (mg), >125–400 mg, and >400 mg, respectively.twenty fiveDuration of MVPA was estimated as the sum of MPA and VPA.
Understanding the results
The primary outcomes of interest in this study were all-cause mortality, cancer mortality, and CVD mortality. Information on date of death and cause of death (ICD-10 C00–C97 for cancer and I00–I99 for CVD) was obtained from death certificates held by the National Health Service (NHS) Information Centre (England and Wales) and the NHS Central Registry (Scotland). The follow-up period began on completion of accelerometry and ended with the occurrence of death or end of follow-up (12 November 2021), whichever occurred first.
Checking covariates
Covariates were selected based on a predefined directed acyclic graph (Supplementary Fig. 3). Finally, our study included age (years from date of birth to start of acceleration measurement), sex (obtained from the central registry at the time of recruitment, field ID: 31), ethnicity, education, smoking status, and alcohol intake (product of frequency of intake and grams of each alcohol per standard drink).33diet quality, sleep quality, self-rated health, history of cancer, CVD, hypertension, long-term illness, disability, frailty, and experience of serious illness, injury, bereavement, stress in the past 2 years obtained from questionnaires, body mass index (BMI, kg/m2A dietary score (0-7) was calculated based on weight (kilograms) divided by height (meters) squared) and waist circumference (centimeters) measured at the first visit, season and wear period recorded by the accelerometer, and diabetes duration (number of years from first onset of diabetes to the start of accelerometer use). A score of 1 was assigned for healthy and 0 for unhealthy frequency of consumption of fruits, vegetables, fish, processed meat, unprocessed red meat, whole grains, and refined grains, with higher scores indicating healthier diet quality.34,35Similarly, a sleep score (0-5) is generated incorporating five sleep factors – chronotype, sleep duration, insomnia, snoring and excessive daytime sleepiness – with higher scores indicating better sleep quality.36.
Statistical analysis
Baseline characteristics of participants according to different physical activity levels were described as means and standard deviations (SD) for continuous variables and numbers (percentages) for categorical variables.
Dose-response relationships of PA with all-cause and cause-specific mortality were assessed using restricted cubic splines fitted to Cox proportional hazards models (the “rms” package in R). The reference value was set at the 1st percentile of the PA distribution, and knots were set at the 5th, 35th, 65th, and 95th percentiles. Potential nonlinearity was tested by Wald tests. Considering current physical activity guideline recommendations (≥150 min/week MPA or ≥75 min/week VPA), the inflection points of the dose-response relationships in our study (approximately 1750, 400, 15, and 375 min/week for LPA, MPA, VPA, and MVPA), and our sample size, we then categorized duration of physical activity into four levels: <1750, 1750–2099, 2100–2449, and ≥2450 min/week for LPA, <150, 150–299, 300–449, and ≥450 min/week for MPA, 0, 1–14, 15–29, and ≥30 min/week for VPA, and <275, 275–449, 450–624, and ≥625 min/week for MVPA. Mortality risk in each group was measured. Cox proportional hazards models were used to estimate HRs and 95% CIs for all-cause and cause-specific mortality risks. Median values of physical activity for each category were entered into the models as continuous variables to examine linear trends. Three multivariate-adjusted models were constructed to account for potential confounders. Model 1 was a crude model adjusted for age (continuous, years), sex (male or female), ethnicity (white or other), education (college or other), season (spring, summer, fall, or winter), and duration of accelerometry (continuous). Model 2 was the main model further adjusted for smoking status (never, former, current, or current), alcohol intake (continuous, grams/day), diet score (categorical, 0–7), and sleep score (continuous, 0–5). Model 3 was an adjustment for BMI (continuous, kg/m2), waist circumference (continuous, cm), self-rated health (excellent, good, fair, poor), long-standing illness, disability or frailty (yes or no), illness, injury, bereavement, stress in the past 2 years (yes or no), history of cancer or CVD (yes or no), history of hypertension (yes or no), and duration of diabetes (continuous, years). In the primary analysis, age, season at time of accelerometer recording, and history of cancer or CVD were treated as time-varying covariates by constructing interaction terms between the covariates and time. The proportional hazards assumption of the Cox model was checked with Schoenfeld residuals and no violations were observed (Supplementary Table 27). Furthermore, we used a risk matrix to explore the joint association of different intensities of physical activity with all-cause and cause-specific mortality. The combination of the least active group was set as the reference group. PAFs were calculated to estimate the proportion of deaths that could be prevented if individuals in the least active group were as active as the most active group.37,38Missing values for covariates with missing rates of less than 1% (e.g., smoking status and BMI) were excluded entirely, and covariates with missing rates of more than 1% (e.g., education and dietary scores) were coded as an additional category for categorical variables or the mean for continuous variables.
Stratified analyses were performed according to age (<60 years vs. ≥60 years), sex (male vs. female), and BMI (<25 kg/m ).2 and ≥25 kg/m2), waist circumference (men <102 cm, women <88 cm, other), smoking status (never, ever), alcohol intake (men <28 g/day, women <14 g/day, other), diet score (<4, ≥4), sleep score (<3, ≥3), and history of hypertension (yes, no) were added to examine whether associations differed by these factors. Interaction terms were tested with Wald tests.
To evaluate the robustness of the results, several sensitivity analyses were performed. First, participants who had cancer or CVD at baseline were excluded when assessing the association between physical activity and the corresponding cause-specific mortality. Second, participants with poor self-rated health were excluded, considering that they were more likely to be physically active and have a higher risk of mortality. Third, to avoid the potential risk of reverse causation, participants who died within the first 2 and 4 years of follow-up were excluded. Fourth, stratified analyses were performed by the number of diabetes severity factors, including glycated hemoglobin level (HbA1c) ≥ 7.0%, diabetes duration ≥ 10 years, and insulin medication use. Fifth, these factors were treated as covariates in the adjustment model. Sixth, T2D-related comorbidities, including associated eye diseases, were also additionally adjusted in the model. Seventh, LPA, MPA, and VPA variables were mutually adjusted to evaluate whether the associations were attributable to the strength of the other. Eighth, cancer deaths were stratified into T2D/obesity-related and T2D/non-obesity-related cancers. Ninth, the main analysis was repeated after imputing missing values of covariates using chained equation multiple imputation (Supplemental eMethods). Tenth, Fine and Gray subdistribution hazard models were used to examine the association between physical activity and CVD mortality, considering cancer mortality as a competing risk. Similarly, CVD mortality was considered as a competing risk when analyzing the relationship between physical activity and cancer mortality through competing risk analysis. Finally, total physical activity, expressed as MET-min/week, was estimated as the sum of the three physical activity modes (LPA, MPA, VPA) according to the International Physical Activity Questionnaire data processing guidelines.39Additionally, we repeated the analysis of all-cause mortality after dividing participants into two groups: those who met the physical activity recommendations in the current guidelines and those who did not meet the recommendations.
All analyses were conducted using STATA 16 statistical software (Stata Corp LLP, College Station, TX) and R software (version 4.1.3). Statistical significance was set as follows: P< 0.05 (two-tailed test).
Report Overview
Further information on the study design can be found in the Nature Portfolio Reporting Summary linked to this article.