Borlaug, BA, Sharma, K., Shah, SJ & Ho, JE Heart failure with preserved ejection fraction: a JACC scientific statement. J. Am. Coll. Cardiol. 811810–1834 (2023).
Borlaug, BA et al. “Obesity and heart failure with preserved ejection fraction: new insights and pathophysiological targets.” Cardiovascular Research 1183434–3450 (2023).
Aryee, E. K., Ozkan, B. & Ndumele, C. E. Heart failure and obesity: the latest pandemic. Prog. Cardiovasc. Dis. 7843–48 (2023).
Aslam, MI et al. Right ventricular sarcomere contractility is reduced in heart failure with preserved ejection fraction and severe obesity. Circulation 143965–967 (2021).
Hahn, VS et al. Myocardial gene expression signature in human heart failure with preserved ejection fraction. Circulation 143120–134 (2021).
Hahn, VS et al. Myocardial metabolomics of failing human hearts with preserved ejection fraction. Circulation 1471147–1161 (2023).
Zile, MR et al. Myocardial stiffening in patients with heart failure and preserved ejection fraction: contribution of collagen and titin. Circulation 1311247–1259 (2015).
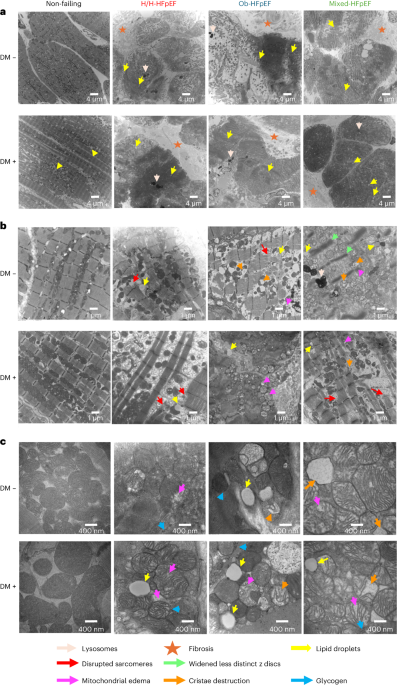
Chaanine, AH et al. Mitochondrial morphology, dynamics, and function in human pressure overload or ischemic heart disease with preserved or reduced ejection fraction. Cardiovascular disease. Heart failure. 12e005131 (2019).
Redfield, MM & Borlaug, BA Heart failure with preserved ejection fraction: a review. JAMA 329827–838 (2023).
Kittleson, MM, et al., “2023 ACC Expert Consensus Decision Pathway: Management of Heart Failure with Preserved Ejection Fraction: Report of the American College of Cardiology Solution Set Oversight Committee.” J. Am. Coll. Cardiol. 811835–1878 (2023).
Anker, SD et al. Empagliflozin in heart failure with preserved ejection fraction. N. Engl. J. Med. 3851451–1461 (2021).
Solomon, SD et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N. Engl. J. Med. 3871089–1098 (2022).
Kosiborod, MN et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N. Engl. J. Med. 3891069–1084 (2023).
Pinto, Y.M. Is heart failure with preserved ejection fraction a metabolic disease? N. Engl. J. Med. 3891145–1146 (2023).
Hahn, VS et al. Endomyocardial biopsy characteristics and prevalence of cardiac amyloidosis in heart failure with preserved ejection fraction. JACC Heart Failure. 8712–724 (2020).
Jani, V. et al. “Role of right ventricular sarcomere contraction inhibition and thick filament activation in human heart failure with pulmonary hypertension.” Circulation 1471919–1932 (2023).
Flam, E. et al. A comprehensive landscape of cardiac metabolism in end-stage human nonischemic dilated cardiomyopathy. National Heart and Vascular Institute 1817–829 (2022).
Schaper, J. et al. Disturbances in myocardial ultrastructure and cytoskeletal changes in dilated cardiomyopathy. Circulation 83504–514 (1991).
Toru Saito et al. “Ultrastructural characteristics of cardiomyocytes are prognostic predictors in dilated cardiomyopathy with early decompensation” Euroheart J. 36724–732 (2015).
Sharov, VG et al. Abnormalities in contractile structure of viable cardiomyocytes in heart failure. International Journal of Cardiol. 43287–297 (1994).
Ahuja, P. et al. “Differential Response of Mitochondrial Biogenesis in Human Cardiomyopathy” Circulation 1271957-1967 (2013).
Collins, H.E. et al. “Mitochondrial morphology and mitophagy in heart disease: qualitative and quantitative analysis using transmission electron microscopy.” Front view. Aging 2670267 (2021).
D’Souza, K., Nzirorera, C. & Kienesberger, P. C. Lipid metabolism and signaling in cardiac lipotoxicity. Biochemistry, Biophysics, Acta 18611513–1524 (2016).
Masayuki Nakamura and Jun Sadoshima “Cardiomyopathy in obesity, insulin resistance, and diabetes” Journal of Physiology 5982977–2993 (2020).
Koleini, N. et al. “Distribution of glycolytic metabolites and their regulatory proteins in the myocardium of patients with heart failure and preserved ejection fraction.” Eur. J. Heart Fail. (In the news).
Maron, BJ, Ferrans, VJ, Roberts, WC Ultrastructural characteristics of degenerated cardiomyocytes in patients with cardiac hypertrophy. Am. J. Pathol. 79387–434 (1975).
van Heerebeek, L. et al. Myocardial structure and function differ between systolic and diastolic heart failure. Circulation 1131966–1973 (2006).
Decker, RS et al. “Myosin-binding protein C phosphorylation, myofibrillar structure, and contractile function during low-flow ischemia.” Circulation 111906–912 (2005).
Ren, J., Wu, NN, Wang, S., Sowers, JR & Zhang, Y. Obesity cardiomyopathy: evidence, mechanisms, and therapeutic implications. Physiology. Rev. 1011745–1807 (2021).
Ritchie, RH & Abel, ED Fundamental mechanisms of diabetic heart disease. Circ. Res. 1261501–1525 (2020).
Chapa-Dubocq, XR, Rodriguez-Graciani, KM, Escobales, N. & Javadov, S. Mitochondrial volume regulation and swelling mechanisms in cardiomyocytes. Antioxidants 121517 (2023).
Weiss, JN, Korge, P., Honda, HM & Ping, P. Role of mitochondrial permeability transition in myocardial disease. Circ. Res. 93292–301 (2003).
Kaasik, A. et al. “Energetic Crosstalk between Organelles: Architectural Integration of Energy Production and Utilization” Circ. Res. 89153–159 (2001).
Burrage, MK et al. “Energetic basis of exercise-induced pulmonary congestion in heart failure with preserved ejection fraction.” Circulation 1441664–1678 (2021).
Sibouakaz, D., Othmani-Mecif, K., Fernane, A., Taghlit, A. & Benazzoug, Y. High-fat diet-induced cardiac biochemical and ultrastructural changes in female and male prepubertal rabbits. Anal Cell Pathology 20186430696 (2018).
Gil-Cayuela, C. et al. Altered expression of autophagy-related genes is involved in heart failure: NRBP2 and Calcoco 2 Correlates with parameters of left ventricular dysfunction in human dilated cardiomyopathy. PLoS One 14e0215818 (2019).
Bozkurt, B. et al., “Epidemiology and Outcome Statistics of Heart Failure: A Report of the Heart Failure Society of America.” J. Card. Failed. 291412–1451 (2023).
Lewis, E. F. et al., “Racial Differences in Characteristics and Outcomes of Patients With Heart Failure and Preserved Ejection Fraction, Heart Failure Treatment with Preserved Ejection Fraction Trial.” Cardiovascular disease. Heart failure. 11e004457 (2018).
Kane, LA, Neverova, I. & Van Eyk, JE Subfractions of cardiac tissue: “In-sequence” myofilament protein extraction from cardiac tissue. Methods Molecular Biology 35787–90 (2007).
Mc Ardle, A. et al. A standardized workflow for accurate medium- to high-throughput proteomics of blood biofluids. Clinical Chemistry 68450–460 (2022).
Robinson, AE et al. Lysine and arginine protein post-translational modifications by enriched DIA libraries: quantification in mouse liver disease. Proteome Research Journal 194163–4178 (2020).
Teo, G. et al. mapDIA: Preprocessing and statistical analysis of quantitative proteomics data by data-independent acquisition mass spectrometry. Proteomics 129108–120 (2015).
Knutsdottir, H. baderzone/HFpEF_2020: Data update (v1.0.1). Zenod https://doi.org/10.5281/zenodo.4287234 (2020).
Kass, D. Myocardial ultrastructure in failing human hearts with preserved ejection fraction. Zenod https://doi.org/10.5281/zenodo.12191847 (2024).