Recognizing the need to predict in-hospital cardiac arrest in critically ill patients, we developed and validated an ML-based predictive model for in-hospital cardiac arrest using HRV measurements in ICU patients. Our model leverages HRV measurements to overcome limitations faced by traditional predictive models that rely on extensive EMR data. The proposed model not only simplifies the prediction process through a single data source but also facilitates real-time continuous monitoring. This result demonstrated the potential of the LGBM model to achieve excellent discrimination performance. This is of paramount importance for early detection and rapid prediction of in-hospital cardiac arrest, thereby improving patient outcomes in real-world clinical settings. This study examines (1) the ability of the proposed model to predict the risk of in-hospital cardiac arrest using only ECG data, (2) the utility of multiple HRV measurements in the proposed ML-based model, and ( 3) It emphasizes the explainability of heart rate variability. Modeling with HRV measurements.
Since this study only used ECG data to predict the risk of in-hospital cardiac arrest, and continuous ECG monitoring is a standard practice in ICU settings, the proposed model is highly accessible. , and can be transferred to other medical settings that collect ECG data. This differs from previous studies that used multiple data sources, such as demographic information, vital signs, and test results, to develop predictive models.4,23,24,25Our model is easily applicable in clinical practice, as only ECG data is required to predict cardiac arrest in the ICU setting. Additionally, we performed a comparative analysis between our model and a clinical parameter-based model from a previous study that utilized 43 features derived from six vital signs. Although the clinical parameter-based model achieved an excellent AUROC of 0.94 in predicting in-hospital cardiac arrest within 1 hour, our findings demonstrate that its performance is poorer when predicting events occurring within 24 hours. showed that it was not consistently maintained (Supplementary Table 1).
Because HRV quantifies dynamic changes in the ECG signal, previous studies have utilized HRV measurements to develop models in various medical situations, including predicting poor outcomes and treatment response.26, 27, 28. However, such studies have used traditional statistical models such as multivariable logistic regression models, and the assumption of linearity between predictors and outcome limits the number of HRV measurements that can be used. Ta.29. In contrast, ML-based models handle complex relationships between predictors and outcomes, so in addition to the traditional set of HRV measurements, the model development process includes other It has the advantage of being able to use a large number of HRV measurements. Mean RR interval (meanNN), SDNN, LF, HF, etc.29. Additionally, ML-based models offer distinct advantages while managing the inherently non-linear and non-stationary fluctuations of HRV measurements.29. In our study, we utilized nonlinear indicators such as IALS, TINN, and HTI, which have been proven to be effective in detecting diseases such as end-stage renal disease, primary hyperaldosteronism, and pulmonary hypertension.30, 31, 32. Integrating these nonlinear HRV measurements into ML algorithms proved to have great potential in achieving superior discrimination performance. This observation was consistent with that of previous studies on various diseases.33which further supports the effectiveness of the proposed approach.
In this study, the BorutaShap algorithm was used to identify the most relevant HRV measurements from 43 HRV measurements, resulting in the selection of 33 HRV measurements as input features for the model. Utilizing such a comprehensive set of HRV measurements improved the accuracy and robustness of the predictive model. Feature importance analysis determined using the SHAP method revealed that TINN, HTI, IALS, Prc20NN, MinNN, and IQRNN were the most important HRV measures in the in-hospital cardiac arrest prediction model.
TINN was the most important feature in our study, followed by HTI. TINN and HTI are both time-domain HRV measurements derived from geometric analysis and provide insight into the overall shape and distribution of the RR interval histogram.Ten. TINN uses triangular interpolation to quantify the baseline width of the distribution of RR intervals. Triangles are determined by least squares error. Generally, a larger TINN value means more variation in the RR interval. Conversely, the HTI reflects the total number of RR intervals divided by the height of these intervals, revealing how the RR intervals are distributed. A lower HTI indicates that a proportion of the interval is concentrated around the mode, and a higher HTI indicates that the interval is more widely spread. Of note, previous studies have emphasized the importance of both his HTI and TINN in cardiac risk assessment. Studies have shown that these values tend to be significantly lower in patients with hypertrophic cardiomyopathy or sudden cardiac death compared to healthy individuals.34. Furthermore, in developing a predictive model for cardiac arrest in critically ill patients, it was found that patients who experienced cardiac arrest had lower TINN and HTI values compared to patients who did not experience cardiac arrest.twenty three. These values also show the differentiation of arrhythmia patients compared to healthy controls, with significant differences in her HTI values between these groups.35. Furthermore, a previous study demonstrated that HTI was an independent predictor of cardiovascular mortality in her AF patients.15.
A new HRV measurement introduced in recent studies was applied in this study. A novel HRV measurement known as heart rate fragmentation (IALS) was identified as one of the key features of our study. For IALS, acceleration and deceleration segments are defined by a set of RR intervals between successive inflection points, and the difference between two RR intervals is <0 および >It was 0. Segment length was determined as the number of RR intervals within that segment.36. Previous studies revealed that IALS was significantly higher in patients with congestive heart failure (CHF), with a mean IALS of 0.78. This result is similar to that of our study (Fig. 5), suggesting that elevated IALS may be associated with worsening cardiac status.37. It is estimated that approximately 30-50% of patients with CHF are at risk of sudden cardiac arrest.38.
Few studies have used other HRV measurements included in our study, such as the IQRNN, to study the relationship between those measurements and cardiac arrest. However, our findings suggested that IQRNN has potential as a predictor of cardiac arrest. The IQRN and TINN values of patients who experienced sudden cardiac arrest remained similar to those of patients without sudden cardiac arrest until approximately 6 hours before the event, after which dynamic changes occurred. Did. Nevertheless, the causal relationship between these HRV measurements and cardiac arrest requires further investigation.
As shown in Figure 5, changes in HRV measurements were analyzed within a time window of 0.5 to 24 hours before in-hospital cardiac arrest and compared with the median values for patients without in-hospital cardiac arrest. IALS values were consistently high. within 0.5 to 24 hours before the cardiac arrest event compared to patients who did not have an in-hospital cardiac arrest. However, these values tended to decrease leading up to the cardiac arrest event. Conversely, HTI values started low but increased toward cardiac arrest. Such continuous changes in HRV measurements have not been documented in previous studies. Therefore, the analytical results of this study are expected to provide valuable insights into the real-time status assessment of patients and facilitate the prompt initiation of interventions aimed at preventing cardiac arrest events.
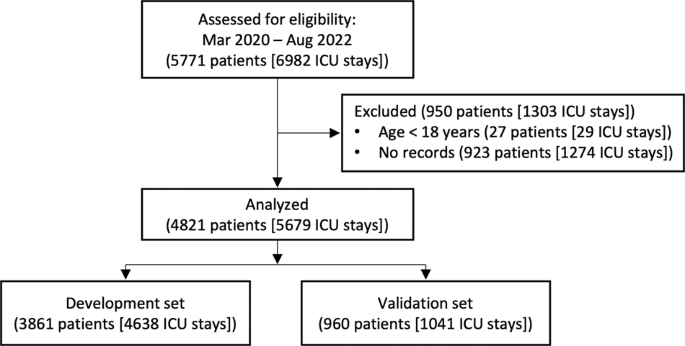
Additionally, this study has the significant advantage of utilizing a large sample size of approximately 5000 patients, increasing the representativeness and generalizability of the results to other patient populations. Large sample sizes are important for accurately detecting rare events such as in-hospital cardiac arrest and are essential for developing reliable ML-based predictive models.39,40.
Nevertheless, the limitations of this study should be considered when interpreting the results. The binary classification model used has certain limitations. This model can only predict whether a patient will experience cardiac arrest; it does not provide information about the timing of cardiac arrest. However, as a side result, we attempted to evaluate the model over different time periods. Additionally, this model does not consider the impact of therapeutic interventions on outcomes and focuses only on baseline predictors. The selection of the development and validation sets may also have been biased, which could affect the accuracy and generalizability of the results. Additionally, this study was conducted in a single center, limiting transferability of the results to other patient populations or health care systems.
Future research should focus on validating the results of this study in larger multicenter studies to increase the generalizability of the results and confidence in the predictions made by the model. Open datasets labeled cardiac arrest and his ECG waveforms, such as the Medical Information Market for Intensive Care, will help validate the results before conducting a multicenter prospective study. Additionally, incorporating clinical factors such as comorbidities and medications could further support the model.41however, we intentionally excluded these factors in this study to account for variation in availability in different hospital settings. Additionally, developing survival models that consider both the probability and timing of cardiac arrest events will provide valuable information for clinical decision-making and improve long-term outcomes for patients who experience sudden cardiac arrest in the ICU setting. We hope that you will be able to understand it deeply. .
In conclusion, we focused on the importance of HRV measures and developed and validated a ML-based real-time prediction model to predict in-hospital cardiac arrest in critically ill patients. If our results are verified in future prospective studies, they may be used to detect in-hospital cardiac arrest in critically ill patients.