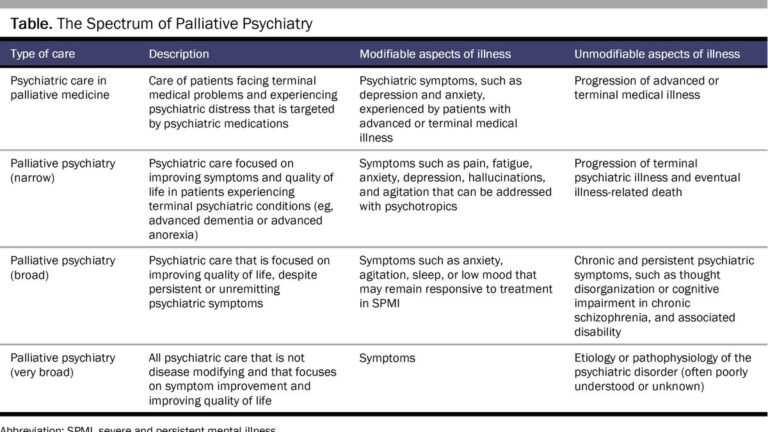
Imagine a field of medicine where the focus shifts from a relentless struggle with symptoms to a compassionate acceptance of living with mental illness, valuing quality of life over active intervention.this is the essence palliative psychiatryThis is a pioneering approach that extends the principles of palliative care, traditionally reserved for terminally ill patients, to those living with severe and persistent mental illness. As we explore this innovative frontier, we uncover the potential of palliative psychiatry to provide comfort, dignity, and a more fulfilling life for individuals who have reached the limits of traditional treatments.
A caring approach to mental health
The beginnings of palliative psychiatry were inspired by Cicely Sanders’ groundbreaking work in hospice care and the concept of “perfect pain.” This research recognizes the multifaceted suffering of patients with serious mental illnesses such as schizophrenia, bipolar disorder and severe depression, whose lives are often overshadowed by the constant shadow of their symptoms. There is. Through palliative psychiatry, a multidisciplinary team of psychiatrists, nurses, social workers, and other health professionals come together to focus on alleviating psychological distress and promoting acceptance of life’s limitations. We provide a comprehensive care plan.
In Canada, the following discussion is taking place: Medical Assistance in Dying (MAiD) Research on people with mental illness further highlights the importance of adopting a palliative approach in psychiatry. This development emphasizes the ethical imperative to explore all possible avenues of care that go beyond mere physical illness and respect the dignity and complexity of human suffering.
Challenges and ethical debates
Despite its promising prospects, palliative care has faced skepticism within the mental health community, due in part to its association with end-of-life care. Critics argue that such an approach could undermine efforts to find effective treatments and lead to a form of therapeutic nihilism. However, proponents stress that palliative psychiatry is not about giving up on patients, but providing more nuanced, patient-centered care that recognizes that traditional interventions may no longer be beneficial. ing.
The introduction of MAiD for mental illness has sparked an ethical debate about the standards and safeguards needed to ensure that MAiD is a genuine option for patients who are in excruciating pain or cannot be cured by other means. This conversation highlights the critical need for a comprehensive palliative care framework in psychiatry that can provide an alternative means of relief and support for people with severe mental illness.
Looking forward: The future of palliative psychiatry
The evolution of palliative psychiatry represents a major paradigm shift toward a more compassionate, patient-centered approach in mental health care. It challenges us to rethink the definition of recovery and success in the treatment of severe mental disorders. By incorporating advanced care planning and emphasizing the importance of patient autonomy and dignity, palliative psychiatry aims to fill gaps in the care of populations that have long been marginalized within the health care system.
As research and practice in this field continues to grow, there is a growing need for collaboration between health care professionals, patients, and families to ensure that palliative psychiatry develops in a way that truly meets the needs of the people it seeks to serve. It is important to encourage dialogue. Although the path to mainstreaming palliative psychiatry may be fraught with challenges, its potential to improve the quality of life for individuals with serious mental illness is a silver lining, and the path to mainstreaming palliative psychiatry is a silver lining. It is a reminder of the profound impact of care.