“What he was most nervous about was the surgery being canceled and the heart not being repaired,” Brown said, a striking contrast to children in the U.S. who have a legitimate fear of the surgery itself. He pointed out that they were doing the same thing.
Now, in an advancement that shows the potential of artificial intelligence to aid medicine, researchers at Children’s National have developed a new AI-powered tool to diagnose rheumatic heart disease long before patients require surgery. was developed. The team worked with staff at the Uganda Heart Institute to design a system that allows trained nurses to screen and diagnose children early. With this system, you can still get penicillin treatment for less than $1 a year. Early treatment could save thousands of people from surgery.
“We focus on dramatically neglected global health issues that cause serious problems. [death and disease],” said Craig A. Sable, Global Health Program Director at Children’s National and one of the authors of a paper describing the AI tool published in the Journal of the American Heart Association.
Sable, who has traveled to Uganda more than 40 times to care for her children, performed eight to nine heart surgeries a week on her most recent trip in November, adding to 1,500 children on the nationwide surgery waiting list. He said he noticed that it was included. .
“Only a quarter of people undergo surgery before dying,” he says.
Difficulty in early detection
Rheumatic heart disease, a largely preventable disease, is caused by the accumulation of repeated bouts of rheumatic fever, which is caused by a bacteria called group A streptococcus. This group of bacteria is considered the fifth most deadly pathogen in the world, with an estimated 600 million people contracting streptococcal pharyngitis each year.
A small number of infected people develop rheumatic heart disease. It is caused by an abnormal immune response that damages the heart and its valves. It is estimated that about 5 to 10 percent of people have a genetic predisposition to this immune response. However, environmental factors such as poor and crowded living conditions also play a role.
Children often show the first symptoms of the disease between the ages of 8 and 10. The disease can be detected early with an ultrasound test of the heart called an echocardiogram. The problem is that countries like Uganda have too few cardiologists who can interpret the images, making widespread screening impossible. As a result, the disease is often undetected in its early stages.
“I don’t know that kid. [they have] that. His parents don’t know about it,” Brown said. “If they go to the doctor, the doctor won’t be able to hear it.”
Rheumatic heart disease plagues poor countries such as Uganda, affecting 2 to 3 percent of all children. Many bacterial strains exist in these countries, and children frequently get repeated infections. The situation worsens with each new match.
The disease is no longer a major problem in the United States, but as Sable well knows, it was very recent in the 1940s and 1950s. He was just a teenager when his grandmother died from complications of rheumatic heart disease and emphysema.
“The heart was the leading cause of cardiac death in the United States in the first half of the 20th century,” Sable said. “More than 100,000 service members were removed from the Army during World War II because of rheumatic fever and rheumatic heart disease.”
AI that “works like a doctor”
The use of artificial intelligence in healthcare has exploded since 2018, when the Food and Drug Administration approved the first independent AI-based diagnostic tool (known as IDx-DR) to screen for diabetic retinopathy. Masu. For diabetics. More than five years later, the FDA has approved nearly 700 artificial intelligence and machine learning-enabled medical devices.
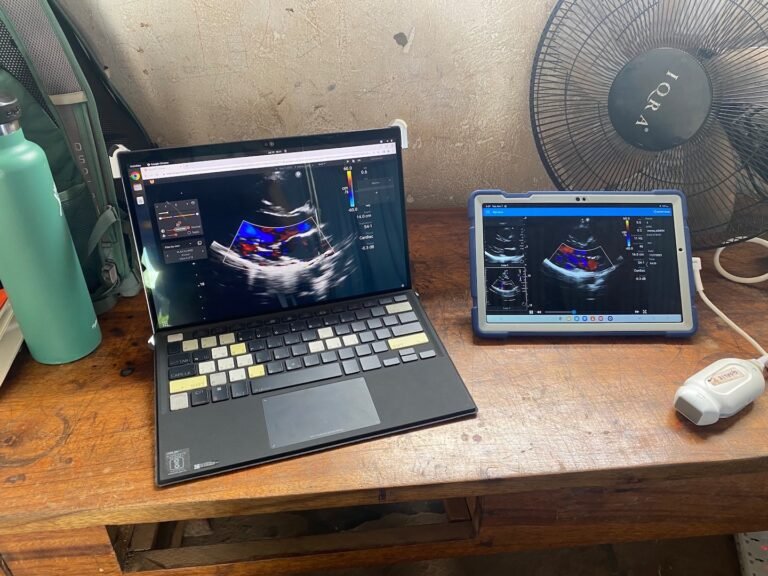
Echocardiography machines in hospitals weigh about 500 pounds and cost $250,000, but the device developed by Children’s National Team is lighter and costs between $2,000 and $5,000. Us2.ai, a Singapore-based company, develops its software using algorithms from a team trained using more than 1,000 echocardiograms.
The algorithm interprets images in seconds and classifies them as either “normal” or “consider rheumatic heart disease.” In testing more than 500 patient echocardiograms, the new tool interpreted images with nearly 90% accuracy.
“If we can use AI to improve the accuracy of images, the value of AI is enormous,” said John, director of the Global Cardiovascular Health Program at the University of Washington, who was not involved in the study. Chris Lonecker said. He said artificial intelligence would make ultrasound a particularly powerful tool because it could be brought “to even the most remote places in low-income countries.”
Lonecker said AI could also help doctors learn more about key features of rheumatic heart disease.
“AI could work like a doctor and potentially add something to what a doctor does,” said Pune Roshanitabrij, a staff scientist at Children’s National. Together with Marius Lingral, a senior researcher at the hospital’s Sheikh Zayed Pediatric Research Institute, he developed a new algorithm for interpreting echocardiograms. Surgical innovation.
Children’s National researchers said the new screening system was tested and refined based on up to 200,000 pediatric cases in Uganda. Each child participating in the program is examined according to current standards with an independent interpretation of the echocardiogram by a trained nurse.
The majority of the data from the 200,000 cases will be used to train and improve the algorithm.
If the new screening tool receives approval from regulators in Uganda and the United States, each nurse will be provided with a probe the size of a computer mouse to generate images of the heart and a tablet with AI components. It turns out.
Cases flagged as possible rheumatic heart disease are followed up with tests by a cardiologist. Cardiologist visits could potentially be conducted using telemedicine rather than requiring travel to and from remote locations.
Shelby Cuti, director of pediatric congenital cardiology at the Johns Hopkins Children’s Center, who was not involved in the project, said similar research has been done on heart disease in adults, but Research in heart disease is relatively limited.”
“Overall, I think this is a very encouraging piece of work,” Kutty added. “I think this area is progressing well.”