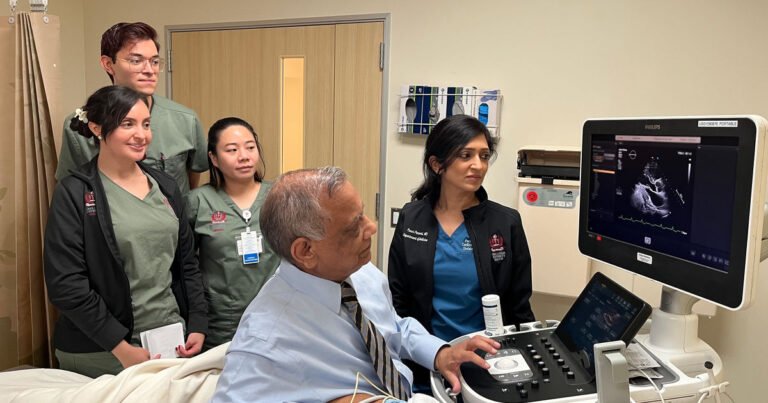
Echocardiography, a noninvasive imaging modality that can provide detailed, real-time images of the heart’s structure and function, has revolutionized the field of cardiology. In the complex world of cardiac care, echocardiography (ECHO) is often a critical first step toward diagnosing, treating and improving a patient’s heart health, says Ramesh Bansal, MD, professor at Loma Linda University School of Medicine and former medical director of the ECHO Lab at the Loma Linda University International Heart Institute.
For decades, the International Heart Institute’s ECHO Lab has played a pivotal role in aiding in early detection and diagnosis, guiding treatment decisions and monitoring cardiac conditions.
“When our team of experts at the International Heart Institute performs echocardiography on patients with complex structural heart disease, it leads to earlier diagnosis, surgical planning and better outcomes,” Bansal said.

Patient Steve Brock, a 63-year-old former firefighter and helicopter pilot, learned about the importance of cardiac imaging using ultrasound after he suffered a life-threatening heart attack. Dr. Bansal first diagnosed Brock with an abnormal heart valve in 1992. An ultrasound scan revealed that Brock had been born with two aortic valves instead of three. If left unmonitored and untreated, Brock’s condition, called bicuspid aortic valve, could cause the aorta, the largest artery in the body, to widen (aortic aneurysm) or tear (aortic dissection).
To avoid this fate, Bansal advised Bullock to get annual echocardiograms. But it wasn’t until 10 years later, in 2003, that Bullock returned to LLUH to be treated for a dangerous aortic dissection. Bullock went into the operating room, where Bansal used an advanced imaging technique called a transesophageal echocardiogram (TEE) to provide cardiac surgeons with critical information about the tear in his aortic valve. Studies at LLUH have demonstrated the benefits of TEE in treating patients with aortic dissection.
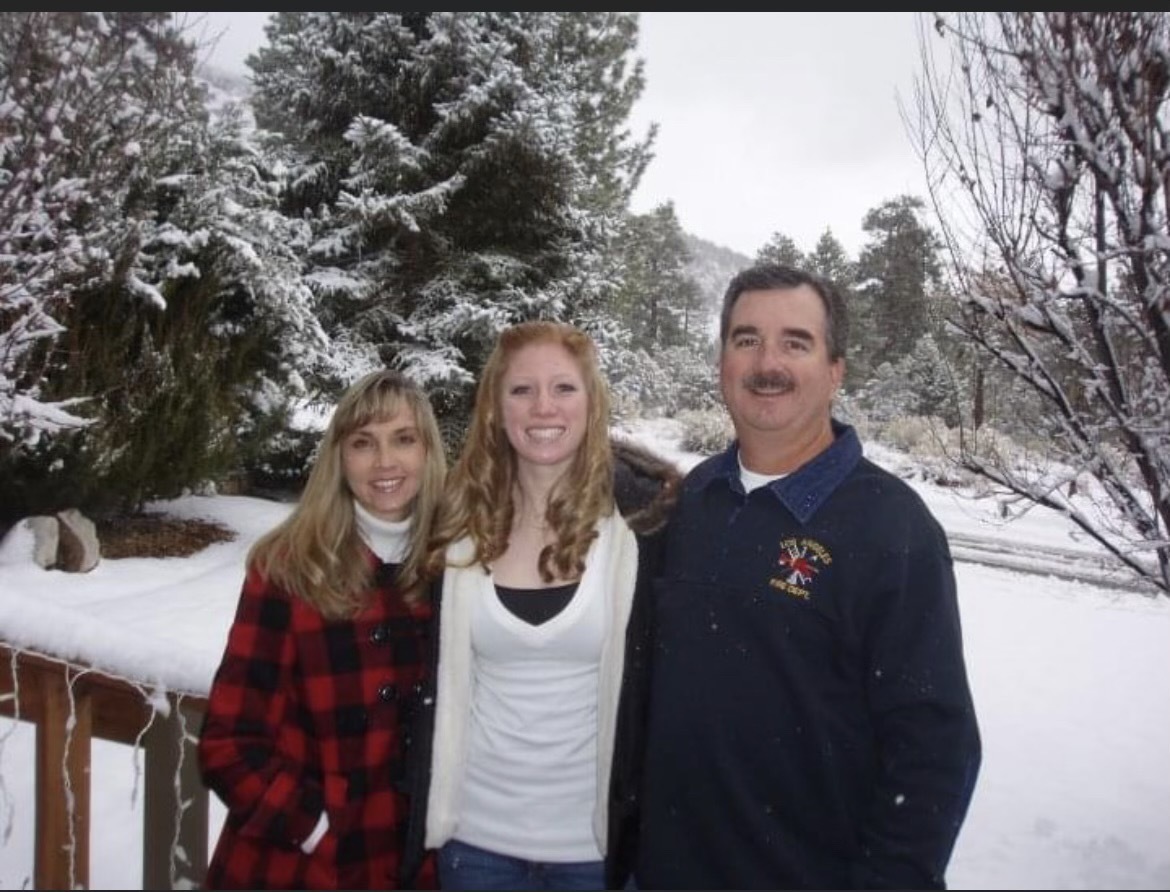
Steve Bullock cherishes the time he spends with his wife, daughter and growing family.
Aortic dissection is a potentially fatal heart condition with an average operative mortality rate of 25 percent, according to data from the International Registry of Aortic Dissection (IRAD). A study of more than 150 patients conducted at LLUH reported that the mortality rate for aortic dissection patients treated at LLUH was less than 10 percent. The International Heart Institute’s multidisciplinary expertise and cutting-edge technology enable the care team to diagnose, treat and cure patients with aortic disease, he says.
Brock has followed Bansal regularly at ECHO since 2003 and is grateful to have been a part of some of his biggest moments, like celebrating his 38th wedding anniversary with his wife, seeing his daughter graduate and watching his granddaughters grow up.
“An ultrasound is very quick, painless and unnoticeable, but it provides valuable information that can prevent someone from having an experience like mine,” Block says.
Bansal says he and other experts at the International Heart Institute are equipped to recognize and treat even the rarest and most complex medical conditions, including congenital heart disease (CHD). In the United States, only 1 percent of babies are born with CHD, Bansal says. With medical advances, more children with CHD are surviving into adulthood, now exceeding 1 million adults, he says, requiring specialized lifelong care and treatment for the condition. Under his guidance over the years, Bansal says the ECHO Institute team has become a leader in the region in caring for the growing number of adult CHD patients.

Leslie Forte has lived with a form of coronary artery disease called Tetralogy of Fallot (TOF) for 35 years. She had her first heart surgery as a baby and began receiving treatment from Dr. Bansal in 2019. Dr. Bansal performed an echocardiogram and discovered a leaking pulmonary valve and a previously unknown hole in her heart called a patent foramen ovale (PFO). She opted for open-heart surgery to repair her heart in 2022, during which Dr. Bansal provided TEE guidance to surgeon Anees Razook, MD, to optimize outcomes.
According to Bansal, cardiac imaging experts play a vital role by providing real-time imaging guidance to medical teams during complex cardiac interventions (such as transcatheter mitral valve end-to-end repair) and surgeries.
“The centre is the only one in the region that can provide A to Z care services to all cardiac patients, no matter how complex their condition,” he said.
read: LLUH Adult Congenital Heart Disease Program Earns Accreditation
ECHO is not only useful in treating valvular and coronary artery disease, but is also essential in diagnosing and monitoring other heart conditions. Brian Kelly has been undergoing regular ECHO testing since 2008, shortly after he was diagnosed with hypertrophic obstructive cardiomyopathy (HOCM). HOCM is a rare, mostly hereditary, condition in which the muscle in the left ventricle of the heart becomes thicker than average and can block the ejection of blood from the heart.

Brian and Jenny Kelly are grateful for the cardiac care they received at the International Heart Institute.
Bansal says the condition puts Kelly at risk for sudden death. He uses ultrasound as an essential tool in risk assessment to analyze high-risk cardiac features, such as the thickness of the heart muscle, the ability of the heart to pump blood (ejection fraction) and the presence of apical aneurysms. Bansal determined that Kelly was at risk for sudden death and recommended that he be fitted with an implantable cardioverter defibrillator to protect his heart from life-threatening arrhythmias.
A few years later, an echocardiogram revealed that Kelly’s thickened heart walls were restricting blood flow, so Kelly underwent a double myectomy to relieve the two-level blockage in her heart. Bansal again provided TEE guidance during the procedure, helping surgeon Razook safely remove Kelly’s blockage.
Genetic testing revealed that Kelly carried a genetic mutation for the disease, which can be inherited, so he and his wife worked with Bansal to have their children tested for the same condition. Both of their children have inherited the disease, and they now undergo frequent echocardiograms to monitor their health.
read: Genetic testing and counseling provide insight into patients’ cardiovascular disease
“We are grateful to Dr. Bansal and his cardiology team for providing our family with the best care over the years,” said Jenny, wife of Brian Kelly, a nurse in the pediatric cardiac intensive care unit. “They are professional, efficient, and use the latest advances in cardiology to care for our family.”
Bansal, who started the ultrasound program at Loma Linda University’s College of Health Sciences, said his students have studied Kelly’s condition as part of their training. Bansal has overseen the growth of the ECHO Lab as its director since 1983, handing the role over to Purvi Parwani, MD, a cardiac imaging specialist, earlier this year, but continues to serve patients and the ECHO Lab himself.
“We pride ourselves on providing the expertise and cutting-edge imaging services to address any cardiac problem, from simple to highly complex,” he says. “At LLUH we offer a range of testing modalities for cardiac patients, including CT and MRI, but it all starts with ECHO. Our number one commitment is to do the best we can for our patients’ health.”
The physicians at Loma Linda University International Heart Institute are committed to providing comprehensive, personalized cardiovascular care for each patient. For more information, visit lluh.org/heart-vascular or call 909-558-7717 to schedule an appointment.